Guidance from the U.S. Centers for Disease Control and Prevention (CDC) on whether COVID-19 patients should stop self-isolating could help the disease spread, doctors have warned. The team in Florida found patients who passed criteria for ending self-isolation were still infected with the virus.
The CDC has two strategies for advising COVID-19 patients to stop self-isolating, one partly based on a negative coronavirus test result, and the second partly based on a patient’s symptoms. The latter approach was formerly known as the “non-test-based strategy” but has been referred to as the “symptom-based strategy” since April 30, 2020, according to the agency’s website.
In a letter to the editor of the Journal of Infection, healthcare providers at a virtual Mayo COVID-19 clinic in Florida warned that based on their experience treating coronavirus patients, “the CDC non-test-based strategy may cause early release from isolation for COVID-19 patients and result in additional community transmission.”
That is because there are a number of unknowns surrounding the coronavirus which is thought to have emerged in China late last year, including how long a person is infectious after their symptoms have passed.
According to the non-test-based strategy, COVID-19 patients can stop self-isolating if they haven’t had a fever for 72 hours without the aid of drugs, their respiratory symptoms have improved, and at least 10 days have passed since their symptoms started. This was increased from 7 days when the guidance was changed on April 30, the authors noted.
In contrast, the test-based strategy involves a patient’s fever passing without the use of drugs, their respiratory symptoms improving, and two consecutive negative coronavirus tests 24 hours apart.
As the Mayo Clinic makes a coronavirus test and the team had “ample testing supplies and laboratory capacity,” they chose to test their patients before telling them to stop self-isolating, and so followed the test-based strategy.
Since April 17, 2020, the team had enrolled 97 patients in its virtual clinic. A total of 72 were tested for the coronavirus after not having had a fever for at least 72 hours, and had 7 days pass since they had their first COVID-19 symptoms. As such, the patients would have met the original criteria for being released from self-isolation.
The team found that the “vast majority” of patients, or 69 percent, tested positive for the coronavirus at this time. A further 22, or 30 percent, tested negative for coronavirus in their first two tests. Of those who tested positive, 36 got that result on the first test, and 14 had their first test come back negative but were positive on the second. On average, it took 19 days for patients to test negative after they first had COVID-19 symptoms.
“Given this, it may be beneficial to prolong the self-isolation time to greater than 14 days after symptom onset,” the team wrote.
Newsweek has contacted the CDC for comment. When the agency updated its guidance to extend self-isolation to at least 10 days it said: “This update was made based on evidence suggesting a longer duration of viral shedding and will be revised as additional evidence becomes available. This time period will capture a greater proportion of contagious patients; however, it will not capture everyone.”
The letter comes as scientists work to shed light on the characteristics of the coronavirus, including how long it lingers in the body, in order to stop it spreading. One study published in the journal the BMJ in late April, for instance, showed coronavirus appears to remain in COVID-19 patients’ stools longer than their respiratory system.
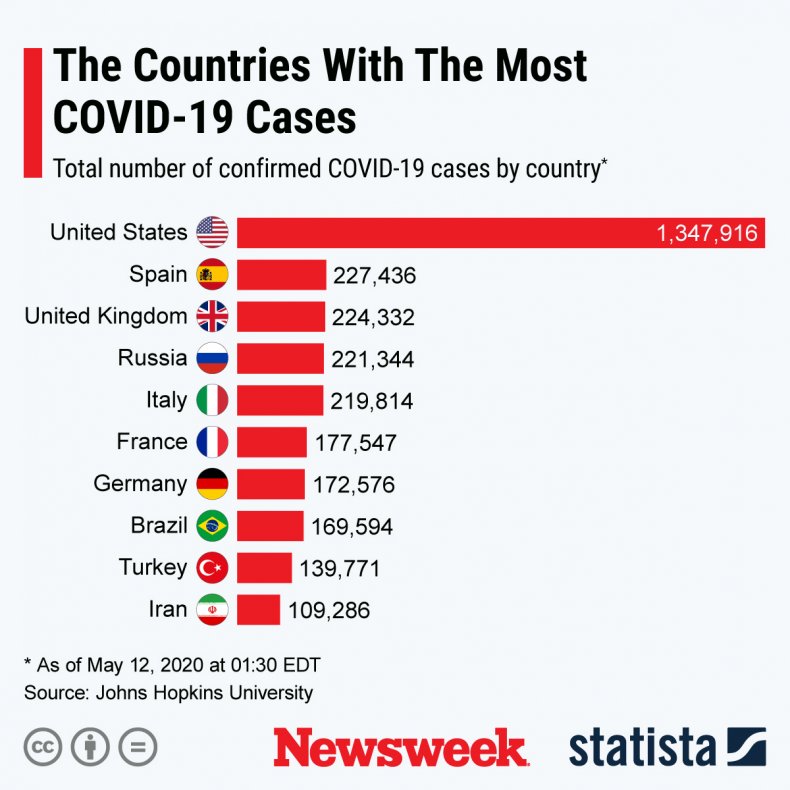
More than 4.2 million people have been diagnosed with coronavirus worldwide, according to Johns Hopkins University. 291,981 people have died, and almost 1.5 million have recovered. The U.S. is the country with the most known cases, as shown in the graph by Statista below.