Coronavirus cases in the U.S. have soared past 7 million to date, with over 200,000 deaths, exactly six months since the country was reported to have the most number of cases in the world.
On March 26, confirmed cases of the virus climbed past 82,000, surpassing that of China and Italy, both of which formerly had the world’s highest number of infections, Reuters reported at the time.
The U.S. was reported to have 86,495 total cases on March 26, according to data compiled by Johns Hopkins University (JHU).
So how did the country get to this sobering ranking and where is it headed? Here we take a closer look at the trajectory of the outbreak in the U.S. and its rapid rise in cases.
Newsweek subscription offers >
CDC believed COVID-19 ‘risk is low’ following first cases
The first case of the virus in the U.S. was reported on January 21 in Washington state and identified to be a person who had traveled to Wuhan, the Chinese city where the virus was first detected.
Days later on January 30, the Centers for Disease Control and Prevention (CDC) confirmed the first domestic case (first instance of person-to-person spread) of the virus in the U.S. The country reported its first infected individual with no history of travel to Wuhan. All prior reported cases were associated with travel to Wuhan.
The infected person was reported to be a resident of Illinois who “shared a household with the patient diagnosed with 2019-nCoV infection on January 21, 2020,” the CDC confirmed at the time.
Newsweek subscription offers >
“Given what we’ve seen in China and other countries with the novel coronavirus, CDC experts have expected some person-to-person spread in the U.S.,” CDC Dr. Director Robert R. Redfield said at the time, adding that “based on what we know now, we still believe the immediate risk to the American public is low.”
That “some person-to-person spread” jumped to more than 86,000 in less than two months from six total confirmed cases reported on January 30, according to JHU.
Average daily new cases in the U.S. remained flat through February. But from mid-March, the average daily case count rose on a sharp incline, according to data compiled by Worldometer.
By March 26, the seven-day moving average of daily new cases was at 10,660. The daily case count first surpassed 10,000 on March 23, according to Worldometer.
A day later, the U.S. became the first country in the world to have more than 100,000 cases. The number of active cases (those currently infected who are in hospital or recovering at home) in the country was reported to be at least 103,847 on March 27, according to Worldometer.
Critical shortage of PPE, ventilators, hospital beds
The risk of spreading infection in the country was amplified by critical shortages of personal protective equipment (PPE), ventilators and other vital medical supplies, which ultimately endangered the lives of both health care workers and the patients who needed them.
On March 21, health workers voiced their concerns to President Donald Trump over the shortages in a joint letter signed by leaders of the American Hospital Association, the American Medical Association and the American Nurses Association.
The letter warned “that increasingly there are dwindling supplies of N95 respirators, isolation gowns, isolation masks, surgical masks, eye protection, intensive care unit equipment and diagnostic testing supplies in areas that had the first community outbreaks and in many other areas of the country.
“Even with an infusion of supplies from the strategic stockpile and other federal resources, there will not be enough medical supplies, including ventilators, to respond to the projected COVID-19 outbreak. We have heard of health care providers reusing masks or resorting to makeshift alternatives for masks,” the letter said.
As cases continued to rise, hospitals faced critical shortages of ventilators and beds and the country was not prepared to cope with the surge in hospitalizations, especially in some of the worst-hit parts of the country in late March, including New York and New Orleans.
New York saw an “astronomical” shortage of ventilators, New York Gov. Andrew Cuomo described at the time.
“It’s not like they have them sitting in the warehouse,” Cuomo said, adding “there is no stockpile available.”
“Any scenario that is realistic will overwhelm the capacity of the healthcare system,” he said at the time.
New Orleans was expected to run out of ventilators by as early as April 2 and reach full bed capacity by April 7, “if we don’t flatten the infection curve soon,” Louisiana Gov. John Bel Edwards warned at a press briefing back in late March.
“It’s not conjecture, it’s not some flimsy theory. This is what is going to happen,” he said at the time.
Back in February, it was estimated that 2.4 million to 21 million in the country could require hospitalization, according to calculations of several worst-case scenarios by the CDC and health experts around the world, which were obtained by The New York Times.
That worst-case scenario would easily overwhelm the 924,107 total staffed hospital beds available in the country, according to the latest data from the American Hospital Association.
Back in March, as many as around a million patients were estimated to require ventilators in a worst-case scenario, according to calculations by Dr. James Lawler, an infectious diseases specialist and public health expert at the University of Nebraska Medical Center, who presented his projections to American hospital and health care executives at an AHA webinar.
The country was reported to have only around 60,000 to 160,000 ventilators available in back in March, according to data from the Johns Hopkins Center for Health Security at the time.
“As the United States braces for a growing wave of patients with Covid-19 in our hospitals and ICUs, we must ensure that we have the key equipment needed to care for patients and to keep our health care workforce safe,” warned a study published in March in the New England Journal of Medicine.
“Failure to act in a coordinated manner would keep many patients from getting the care they need and would lead to the situation we see in Italy, in which frontline clinicians are making difficult decisions about who will and who won’t receive care.
“Furthermore, without adequate PPE, health care workers will get sick, endangering the functioning of the entire health care system. The human and economic costs of that scenario should not be underestimated,” the study added.
Lack of testing
Increased testing and monitoring the percentage of positive cases (the positivity rate) in a given population are crucial elements of mitigating the spread of infection.
“As testing capacity increases, considering confirmed new cases, testing rates, and percent positivity together gives us a fuller picture of COVID-19 in a particular state or region,” JHU explained.
“Under these conditions and stable testing practices, trends in daily cases can be cautiously interpreted as trends in transmission of the virus. Leaders can then make informed decisions about lifting social distancing and other transmission control measures,” JHU noted.
Back in March, when asked to comment on the fact that the U.S. had surpassed China and Italy with the most number of cases in the world, President Trump said at a White House press briefing: “I think it’s a tribute to our testing. We’re testing a tremendous number of people.”
By late April, less than a month since the U.S. hit the milestone, only around one percent of the American population had been tested for the virus.
At least 4,163,464 people in the U.S. were reported to have been tested, as of April 22. This amounts to around 1.2 percent of the country’s population of nearly 332,639,000.
New York, the worst-hit state, had tested around three percent of its more than 19.5 million residents, with nearly 650,000 tested as of April 22.
Less than one percent—nearly 0.7 percent—of the population of California (nearly 39.5 million), the country’s most populous state, were reported to have been tested as of April 22.
Speak to Newsweek, Dr. Anthony Fauci, the director of the National Institute of Allergy and Infectious Diseases and member of the White House COVID-19 task force, previously said: “We need to do better [with testing]… we need a well-organized system at the state, city and local level, with guidance and help from the federal government, to be able to have enough tests as cases begin to resurge.”
Fauci warned the country needs “to have in place the system, the test, the capability, the manpower to do the kind of identification, isolation and contact tracing as cases begin to reappear in the fall, because they will reappear.
“For the kind of contact tracing that needs to be done, you need manpower. You need people who can be mobilized efficiently to do the kinds of contact tracing we need. If we have that, we could avoid a resurgence or what people would be calling a second wave,” he said.
Most COVID-19 deaths in the world
By late May, the U.S. death toll surpassed 100,000 and led the world with the highest number of COVID-19 fatalities, jumping from less than 2,000 total deaths reported a couple of months prior when it was reported to have the most confirmed cases in the world, according to JHU.
Average daily new deaths in the country have been increasing from late March to April 17, when the average daily death count peaked at 2,248. It then briefly flattened out until late April and mostly declined through early July, according to Worldometer.
From around July 4, the average daily death toll increased through early August, but not at the higher levels seen in April and May. The figure then decreased through early September before flattening out through the rest of the month, according to Worldometer.
Earlier this week, the death toll doubled to over 200,000, marking yet another grim milestone.
Where we are now
After increasing sharply from early June, the average daily case count in the U.S. declined through late August before flattening out through September. The average daily death count has been flattening out from late May, according to the data from Worldometer.
Average daily new cases in at least 25 states were reported to be on an upward trend in the latest two-week period from September 10 to 23, according to the latest report Friday by JHU.
Back in May 12, 2020 the World Health Organization (WHO) advised governments that “before reopening, rates of positivity in testing (ie, out of all tests conducted, how many came back positive for COVID-19) should remain at 5 percent or lower for at least 14 days,” JHU noted.
“Ideally, a state should be meeting or exceeding the recommended positivity rate, which the WHO has set at 5 percent. A positivity rate over 5 percent indicates a state may only be testing the sickest patients who seek out medical care, and are not casting a wide enough net to identify milder cases and track outbreaks,” JHU explained.
Currently, 25 states are reported to meet the WHO’s positivity rate recommendation, according to the latest report Friday by JHU.
Average daily deaths have also flattened out from early June through September, after peaking in late April, according to Worldometer.
But the total death count is projected to climb to 425,919 by January 1 with “continued easing of social distancing mandates and mandates are not reimposed,” according to the latest projection from the Institute for Health Metrics and Evaluation (IHME).
The U.S. currently has the sixth highest death rate of 61.99 deaths per 100,000 people among the 20 countries “currently most affected by COVID-19 worldwide,” the latest report Friday by JHU noted.
According to the aforementioned estimates of the worst-case scenario by the CDC and global health experts, around 160 million to 214 million people in the U.S. could be infected over the course of the pandemic.
“There’s no doubt that this virus is not going to disappear from the planet by the time we get to the fall and the winter,” Fauci told Newsweek in late May.
“It’s in our hands. We can prevent a second wave if we respond to the inevitable infections we’ll see in the fall and winter.
“When those inevitable cases appear, it doesn’t mean we inevitably will have a second wave. It’s about how we respond to prevent these infections from becoming a true resurgent wave. It’s in our hands, we’ve got to be able to grab the bull by the horns and be prepared,” Fauci warned.
The wider picture
The novel coronavirus has infected over 32.5 million people across the globe since it was first reported in Wuhan, China, including over 7 million in the U.S. More than 988,900 have died following infection, while over 22.4 million have reportedly recovered as of Saturday, according to JHU.
The graphic below, provided by Statista, illustrates U.S. states with the most COVID-19 cases.
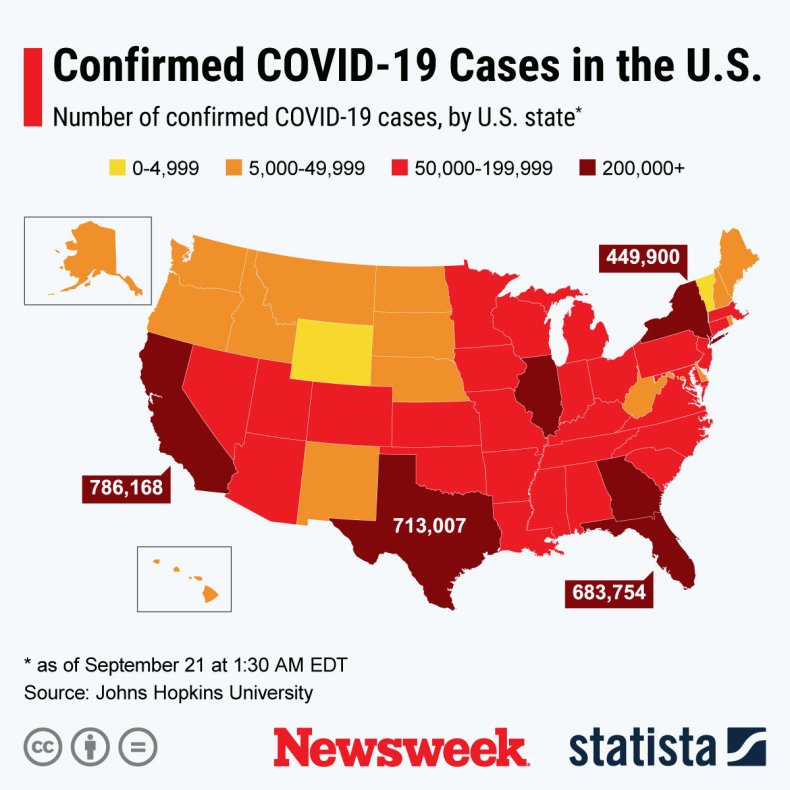 STATISTA
STATISTAThe below graphic, also provided by Statista, illustrates the percentage of Americans who do or don’t want COVID-19 restrictions to be relaxed in the country.
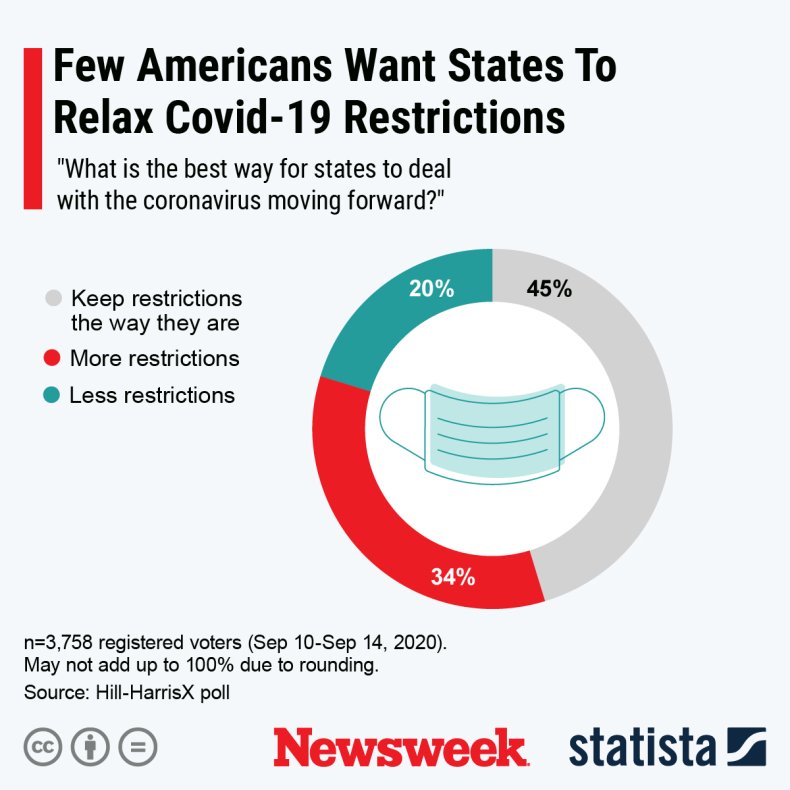 STATISTA
STATISTAThe graphics below, also provided by Statista, illustrate the spread of COVID-19 cases in counties across the globe.
1 of 2
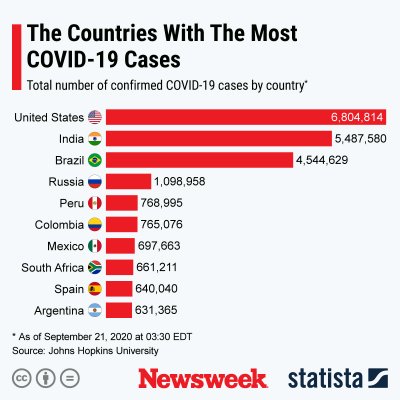 STATISTA
STATISTA STATISTA
STATISTA 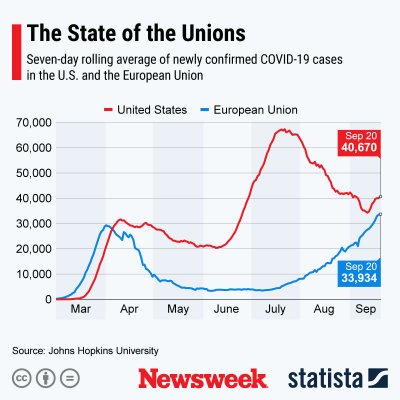 STATISTA
STATISTA


















